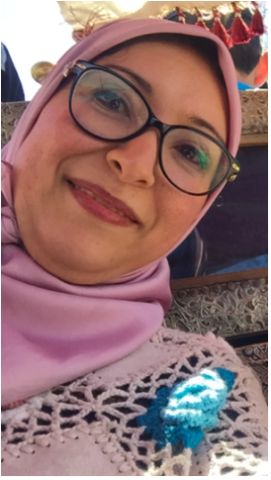
Meet Dr Ibtissam Khoudri from Morocco’s Ministry of Health
Interviewed by Jessica Cook and Andie Tucker, Global Partnership for Zero Leprosy Communications
Dr Ibtissam Khoudri leads the leprosy programme in Morocco’s Ministry of Health and is a chairperson for the Operational Excellence working sub-group 5 on infrastructure and operational capacity. The communications team from The Global Partnership for Zero Leprosy (GPZL) spoke to her about Morocco’s success in reducing leprosy, the critical issues countries face in trying to get to zero leprosy, and how the partnership’s work can help.
What is your background and how did you come to work in the field of leprosy?
I am a dermatologist and also have degrees in epidemiology and biostatistics. I worked as a dermatologist in an endemic area of Morocco and then moved to the Ministry of Health, where I have been leading the leprosy control programme for the last six years.
As a dermatologist, did you see many patients with leprosy?
I was working in an endemic area in Morocco, so in this city we had cases of leprosy. Overall, Morocco is a low-endemic country, so I saw about five cases per year. During that time, I also had experience doing contact surveillance. We had a strong system of contact surveillance there.
Since 2012, the number of cases of leprosy in Morocco has declined by more than 16 percent per year. What do you think is the key to Morocco’s success?
In the last several years, Morocco invested in a strong surveillance system, which is better at following up with new cases. Contact tracing is one explanation for Morocco’s success. At a national level, we have been implementing single-dose chemoprophylaxis for household contacts since 2012, and in the last year, demonstrated a clear decline in the number of new cases.
Also, since the implementation of WHO’s protocol in 2006, our government has made significant changes, allowing for better geographical access to health care, early case detection and treatment, and a long duration of treatment. The training of health care workers and the integration of leprosy control services in primary health care services has helped a lot. The improvement of socio-economic conditions has also helped reduce leprosy here.
You lead the Operational Capacity sub-group in our Operational Excellence working group. What kind of work is the group doing?
Our group looks at cross-cutting issues in leprosy, like human resources, finance, evaluation, surveillance and policy. We’re developing a list of best practices that can really help countries that want to move to zero leprosy.
Sharing experiences — real and practical experience from countries — is needed.
There is a need to identify practices that have demonstrated results and to share them with each other.
What do you think are the most important issues for national program managers in leprosy?
The big issue is how to make early detection of cases possible, and putting a system in place that can follow up with registered cases. More than 60% of new cases are from household and neighbour contacts in Morocco. We need to follow-up with contacts to detect new cases early and help people get treatment. It would also be helpful to document any cases of antibiotic resistance.
The Global Partnership for Zero Leprosy will partner with national programmes on country reviews and road maps. How can we best support national programmes?
The country reviews and the creation of strategic road maps are important for high- and low-endemic countries. For a low-endemic country like Morocco, leprosy is no longer a priority, yet the country still is not at zero leprosy. In situations like this, we need to show national governments how we can maintain activities, perhaps integrating these activities in other NTD programmes. The road map can make clear the activities that are still needed and can give direction for next steps. The ambition is there—we all want to move toward zero—but how? It’s not always clear for countries. This is what the country review and road map can provide.
Reposted with permission from The Global Partnership for Zero Leprosy – originally published 6 May 2019 here.