Global Leprosy Update 2019
Commentary by the ILEP Technical Commission, September 2020
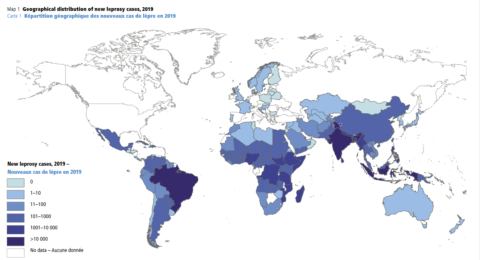
This new update presents a large amount of helpful data on the present state of leprosy around the world, generally in Tables whose format we have become used to. An Editorial comment at the end gives further perspective. The data themselves were received from 160 countries through the DHIS2 software or through an Excel-based form, which holds the promise of gradually improving consistency in the coming years.
The sub-title, “Time to step-up prevention initiatives” is the main focus of the Editorial comment on the last 3 pages, emphasizing the Triple Zero targets. Post-exposure prophylaxis (PEP) with single-dose rifampicin is mentioned as a WHO recommendation, but there are no process indicators in the report which would help to monitor progress. There are many possible indicators, such as the number of countries with a policy to implement PEP, or the number of contacts who were given PEP. Work is underway to estimate the population requiring PEP globally, so it would be worthwhile to start collecting data about how many people are receiving it. Along side PEP indicators, WHO also recommends monitoring trends in rifampicin resistance, which could theoretically be affected by PEP.
The main leprosy indicators are now all based on a denominator of 1 million population (1 million children, in the case of rates in children) and this standardization is welcome; it also helps to suggest that calculating these indicators for small populations may be misleading. The key indicators are the case detection rate, the disability rate and the case detection rate in children. The rate in children is declining gradually (7.78 per million children in 2019) and the 2030 target is to be below 0.8 cases per million children: this will be a challenge, but the indicator seems robust and helpful; it remains our best estimate of recent transmission. The main problem with the figure of 7.78 per million children is that it conceals a very wide range of results for individual countries and regions (See Table 1 below). It would be useful to see this rate presented in future for each of the 23 global priority countries, with trends over time. Larger countries may also find regional trends useful in identifying areas of higher endemicity.
Table 1: Case detection rate (CDR) in children for 23 priority countries, per million children. For countries with < 1m children, the exact rate is not calculated, but it is very high. Data are taken from Table 5 of the Global Leprosy Update for 2019. The CDR is calculated from the first two columns of data (b/a).
|
Country |
a. Child population (millions; 2019) |
b. Child leprosy (2019) |
CDR in children (=b/a) |
| 1 |
Angola |
12.985 |
116 |
8.93 |
| 2 |
Bangladesh |
45.318 |
210 |
4.63 |
| 3 |
Brazil |
45.762 |
1545 |
33.76 |
| 4 |
Comores |
0.305 |
270 |
> 100 |
| 5 |
Côte d’Ivoire |
9.723 |
44 |
4.53 |
| 6 |
Dem. Rep. of the Congo |
34.659 |
158 |
4.56 |
| 7 |
Egypt |
30.716 |
26 |
0.85 |
| 8 |
Ethiopia |
42.075 |
507 |
12.05 |
| 9 |
India |
370.183 |
7859 |
21.23 |
| 10 |
Indonesia |
70.601 |
2009 |
28.46 |
| 11 |
Kiribati |
0.037 |
37 |
> 100 |
| 12 |
Madagascar |
9.996 |
96 |
9.60 |
| 13 |
Micronesia (Federated States of) |
0.035 |
46 |
> 100 |
| 14 |
Mozambique |
12.156 |
211 |
17.36 |
| 15 |
Myanmar |
14.429 |
105 |
7.28 |
| 16 |
Nepal |
8.876 |
293 |
33.01 |
| 17 |
Nigeria |
77.616 |
276 |
3.56 |
| 18 |
Philippines |
32.767 |
99 |
3.02 |
| 19 |
Somalia |
6.326 |
35 |
5.53 |
| 20 |
South Sudan |
4.12 |
120 |
29.13 |
| 21 |
Sri Lanka |
5.075 |
176 |
34.68 |
| 22 |
Sudan |
15.913 |
13 |
0.82 |
| 23 |
United Republic of Tanzania |
22.712 |
53 |
2.33 |
The Grade 2 Disability (G2D) rate is gradually declining, but it is questionable whether the 2020 target of < 1 per million population will be met. In Table 4 it would be helpful to add one line at the bottom, below the total new cases with G2D, giving the rate per million. Small changes from year to year are less significant than longer term trends, but the increasing number of new cases with G2D in Brazil over the past 5 years, as shown in Table 4 of the Update, is a concern. Although the Covid pandemic of 2020 does not affect these 2019 data, the capacity of health services to provide an acceptable level of care to those in need may be impaired in the coming years.
There are sparse data available for several issues that are mentioned briefly. Antimicrobial resistance (data from 11 countries), reactions (19,590 cases in 41 countries), adverse events related to MDT (none reported), foreign-born cases (836 individuals in 37 countries, of which 11 countries had no indigenous cases), relapse (3893 cases) and retreatment (15,517 cases). It is commendable that these data are now being collected and in future, it will be interesting to watch historical trends and to analyze individual country data in more detail. As almost 80% of all retreatment cases were reported from Brazil and India, it is vital that monitoring antimicrobial resistance is reinforced in those countries.
The number of countries with discriminatory laws was 22 despite recent efforts. In the field of psychosocial support to people affected, new indicators are needed, but the relevant data may be difficult to collect. Access to effective counseling is one area that could be monitored.
There are a few typing errors: in Table 2 the 2019 figure for cases with G2D in SEA is written as 817, but it should be 4817, as indicated elsewhere in the report. In Figure 2, the legend describes the chart as depicting trends in the case detection rate among children, whereas it actually shows the numbers of cases, not the rate; the description of Figure 2 in the text is correct. In the last paragraph on p424, the first sentence seems to be incomplete.
In conclusion, the update presents a wealth of data which will be useful to policy-makers, planners and researchers everywhere. The emphasis on stepping up preventive activities is welcome. Data allowing anyone to calculate the CDR in children in any country, is useful to indicate the underlying level of ongoing transmission, but in future, indicators to monitor the implementation of PEP will be needed. Data on issues such as drug-resistance, reactions, relapse, retreatment and adverse events are being collected, but at present are not complete enough to draw meaningful conclusions. The basic indicators on disability (G2D rate, and the rate in children) and discrimination (remaining discriminatory laws) should be complemented by indicators that monitor both disability management and steps being taken to reduce stigma, at community level, as proposed in the Global Leprosy Strategy 2021-2030.